Leveraging data for better healthcare quality measures
Quality measures are a cornerstone of value-based care, and data helps organizations audit and improve their economic and medical performance
Quality measures are a cornerstone of value-based care, driving the pursuit of higher standards and improved patient outcomes. As healthcare executives and experts strive to enhance the performance of providers and organizations, data has taken center stage in this mission. In a recent discussion at HIMSS 2023, Arcadia’s Senior Customer Success Manager Zach Blecher and Director of Enterprise Partnerships Nick Kamireddy discussed the critical role of data in refining quality measures, shedding light on how real-time insights revolutionize the way healthcare organizations approach their contracts and patient care.
Data’s the difference-maker for quality improvement
Quality measures constitute a pivotal facet of value-based care, but to accurately gauge what’s happening within a healthcare organization (much less improve results), it’s critical that data gets surfaced quickly and efficiently. This is where technology can elevate healthcare systems above the other players in the field.
Arcadia’s data analytics platform relies on a steady influx of data — from claims to clinical records and supplementary lab data — all meticulously synthesized into actionable insights. Unlike traditional methods that often rely on outdated or limited data, Arcadia's measures engine thrives on the integration of real-time clinical data, offering a dynamic view of an organization's performance.
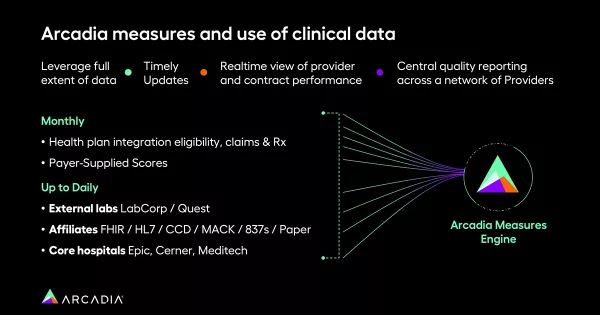
“We rely heavily on data from across your network. That includes claims data, which comes in usually about monthly; clinical data, which we ingest up to daily from any of your EHR sources; and then we get supplemental lab data,” Blecher explains. “All of that data then gets ingested into what we call our measures engine, and that measures engine outputs the results of the measures.”
The implications of this approach extend beyond mere convenience. Timely and accurate data fuels performance improvement plans and strategic decision-making. By harnessing real-time insights, organizations are empowered to identify challenges, anticipate risks, and address gaps swiftly. This proactive stance, fortified by data-backed insights, not only bolsters a provider's ability to attain higher star ratings but also enhances patient care through more targeted and informed interventions.
“Staying at a four- or five-star performance level for a lot of measures requires that you have some of those supplemental data points that payers don't always get on their own,” Kamireddy emphasized. “Through clinical data integration, we can see that more real-time performance.”
“Being able to help support that through more real-time data is critical to overall performance as well as their satisfaction,” he said.
Building a data-driven provider-payer partnership
The integration of clinical data ushers in a new era of provider-payer collaboration. Blecher and Kamireddy underscored the importance of providers having access to timely data that accurately reflects their actions and patient care efforts. This fosters trust in data accuracy, streamlining the provider's focus on care delivery rather than reconciling discrepancies.

“As we think about the transition to value-based care, it's really kind of held back by a provider's ability to feel comfortable with what they're going to be managed against in those contracts,” Kamireddy said. “You can build that confidence to say, ‘You know, you're really doing better than you think! Moving to value-based care isn't going to be as painful as you expect that it could be.’”
Furthermore, timely clinical data paves the way for meaningful patient outreach, ensuring that patients are engaged promptly based on the latest information, ultimately improving care quality. The proof is in successful campaigns, like the ones many healthcare organizations have undertaken to increase medication adherence. By scrutinizing pharmacy claims and monitoring adherence in real-time, healthcare organizations can tailor outreach efforts to prevent patients from falling out of compliance. This approach not only advances patient outcomes but also showcases the potential of data in driving proactive interventions.
Additionally, the integration of clinical data serves as a catalyst for clinical data-driven quality incentive programs. The consolidation of disparate data sources into a single platform empowers organizations to streamline performance improvement initiatives and achieve a deeper understanding of their provider network's performance. This, in turn, bolsters relationships between healthcare organizations and payers, driving positive outcomes and positioning for future collaborations.

The future of care, illuminated by data points
Data’s a pivotal tool in the quest to enhance healthcare quality measures. The integration of real-time clinical data not only revolutionizes the accuracy and timeliness of performance insights but also cultivates a culture of proactive care delivery. As healthcare executives and providers forge ahead in their pursuit of improved patient outcomes, the power of data-driven quality measures is a beacon guiding the way toward a more effective, efficient, and patient-centered landscape.
Want to leverage data and watch your performance skyrocket? Watch a demo to see how an analytics platform gives payers an edge.
